Burr hole evacuation for infratentorial subdural empyema
07/06/2019The role of computed tomography in detecting splenic arteriovenous fistula and concomitant atrial myxoma
The role of computed tomography in detecting splenic arteriovenous fistula and concomitant atrial myxoma Arben Rroji,A,B,D,E,1 Fatmir Bilaj,A,B,D,E,1 Denis Qirinxhi,B,E,F,1 Ortencia Vucini,B,D,E,2 Endri Hasimi,B,D,E,2 andArtan GodaA,B,E,2
Abstract
Patient: Female, 45
Final Diagnosis: Arterio-venous fistula of the splean
Symptoms: Lef-side abdominal pain
Medication: —
Clinical Procedure: —
Specialty: Surgery
Objective:
Rare disease
Background
A splenic arterial-venous fistula (SAVf) is caused by an abnormal discharge of the distal splenic artery into the corresponding vein. This pathology should be especially suspected in cases when patients complain of a vague left flank pain associated with a loud murmur, or acute portal hypertension not related to chronic liver disease. They may be asymptomatic or lead rapidly to the development of portal hypertension [1,2].
Myxoma is the most common benign tumor of the heart. It is found accidentally, as in this case, or could present with various clinical signs [3,4]. To the best of our knowledge, SAVf with concomitant atrial myxoma represent a unique pathology, previously unreported in the literature. Go to:
Case Report
A 45-year-old woman presented with a vague left flank pain. The pain started 3 years ago but became more persistent and was associated with a loud pulsatile murmur. The patient was a well
nourished Caucasian female. The liver was not palpable and no signs of jaundice were observed. The rest of the physical examination was unremarkable. Heart rate was regular and rhythmic. Blood pressure was 110/80 mm Hg. The liver and kidney test results were normal, and the rest of laboratory test results were unremarkable. An ECG revealed normal sinus rhythm. The patient had no prior history of abdominal trauma, accidental injury, or abdominal surgery.
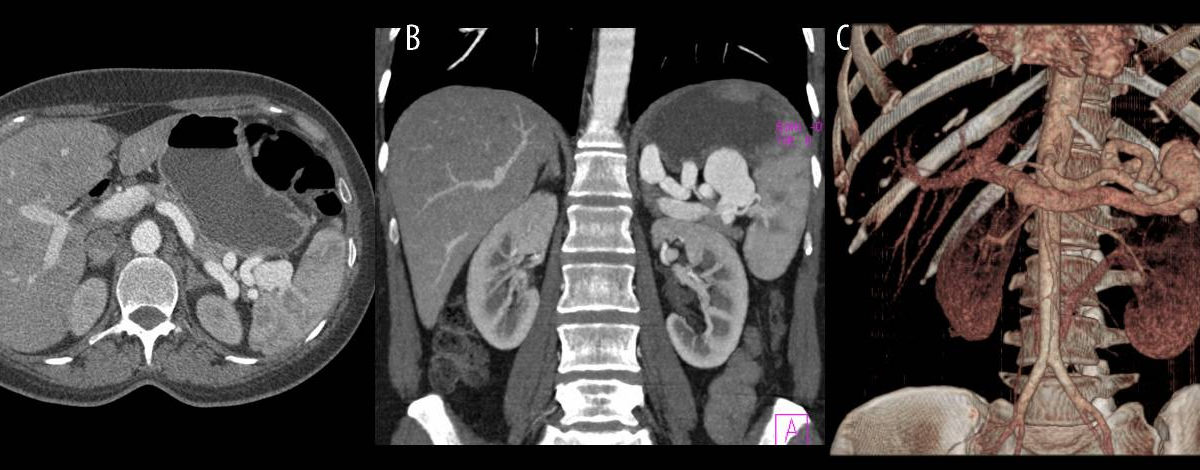
Abdominal echography showed multiple round hypo-echoic lesions in the splenic hilum, most likely representing dilated splenic vessels. CTA revealed a tortuous dilated splenic artery and aneurismal dilatation of the splenic vein associated with an early opacification of the portal system. The dimensions of the aneurysm were: cranial-caudal 57 mm, latero-lateral 43 mm, and antero-posterior 24 mm. CTA also showed an intrasplenic venous aneurysm, which was presumed to be the location of the fistula (Figure 1A–1C).
Figure 1.
(A) Axial computed tomography in the arterial phase showed dilatation of splenic artery, aneurismal dilation of the splenic vein, and small intra-parenchymal splenic aneurysm. (B, C) Reformatted maximum intensity projection (MIP) and volume rendering techniques (VRT) images in the coronal plane showed tortuous dilated splenic artery and multiple aneurismal dilatation of the splenic vein.
Celiac and splenic arteriographies were carried out and showed a tortuous splenic artery with a large venous aneurysm combined with premature portal and splenic vein filling and marked opacification of the spleno-portal axis (Figure 2A, 2B).
Figure 2.
(A, B) Angiography showed a splenic arteriovenous fistula.
The patient was seen by the cardiologist to evaluate potential complications from SAVf. The cardiologist noticed that the patient had non-frequent palpitations, effort dyspnea, but no chest pain and normal cardiac function. Transthoracic echocardiography showed a large mass in the left atrium. Subsequently, the patient had a cardiac CT, which showed a large mass arising from the inter-atrial septum and protruding towards the mitral valve, consistent with atrial myxoma (Figure 3A, 3B). Based on the presence of both pathologies, surgical treatments were required.
Figure 3.
(A, B) Computed tomography showed a large atrial mass protruding towards the mitral valve.
Initially, the patient underwent a successful cardiac surgery. During the operation, a large mass was identified attached to the septum of the left atrium with a thin peduncle that measured approximately 1 cm. The mass was removed and the defect in the atrial septum was covered with an autologous pericardial patch. Several weeks after the cardiac operation, the patient underwent laparotomy with dissection of SAVf and splenectomy. The postoperative period was uneventful in both cases. After several months of follow-up, the patient was doing well and did not present any complaints.
Discussion
SAVf was first described by Wiegert in the 19th century. Atrial myxoma is the most common type of benign cardiac tumor in adults. The literature does not reveal any connection between these 2 entities and we speculate that they are separate diseases, which were diagnosed at the same time. Further studies would be helpful to explore a possible connection between these 2 pathologies. The mechanism of SAVf formation is an abnormal route of communication of a splenic artery aneurysm (SAA) with the corresponding vein. The predisposing factors for arterial aneurism are increased blood flow and arterial wall damage associated with weakness of the smooth muscle layer. The cause can be congenital, infectious, due to pancreatitis, acquired after trauma or accidental penetrating injury, and prior surgery in the abdominal cavity. It is more common in multiparous women than in men, with a sex ratio 4 to 1 [1,2]. SAVFs may stay clinically silent for a long period of time. When the aneurism is formed, the patient complains of discreet pain and bruit in the left flank, as observed in our patient.
Myxoma is mostly located in the left atrium, but in rare cases it is encountered in the right atrium. There is a recognized female predilection. The clinical presentation is variable; approximately 20% of myxomas are asymptomatic, or have general symptoms like weakness and weight loss. Depending on the degree of prolapse of the mass into the mitral valve, it could be associated with valvular obstruction, arrhythmia, or embolic diseases, particularly in the brain. The myxomas of the right side of the heart present with symptoms of heart failure. As the number of imaging diagnostic procedures is increasing, more myxomas are accidentally detected. They may be associated with multiple endocrine neoplasia (MEN) syndromes, known as the Carney triad [3,4].
The hemodynamic changes in SAVf may lead to a sudden increase of portal venous pressure, which is manifested with gastrointestinal bleeding, varices, and ascites. Portal hypertension due to chronic liver disease usually requires a longer period of time. Increased portal pressure is associated with splenomegaly and other gastrointestinal signs [5,6]. This patient had a normally sized spleen and liver. The liver had no parenchymal changes and the portal vein was normal.
Cardiac symptoms have been reported by Gunther and include tachycardia, left ventricular dilatation, and ischemic disease of the myocardium [7]. Our patient had some cardiac symptoms that were more related to atrial myxoma.
Vague pain in the left flank was the most persistent symptom in our patient. She started complaining 3 years ago, but because of the vague nature and undetermined echographic findings, she had not been diagnosed. The estimated risk of rupture depends on the size of the aneurysm. There is an increased risk during pregnancy, but this was not the case for our patient [8].
Her past medical history was uneventful. Besides past pregnancies, we did not find any cause to speculate about the origins of this SAVf.
The CTA imaging findings were straightforward in both SAVf and atrial myxoma. The differential diagnoses of primary atrial mass include fibroelastoma, rhabdomyoma, fibroma, lymphoma, and sarcoma. Rhabdomyoma and fibroma mostly affect children, and the other tumors have different clinical and morphological features [9]. Nowadays, the treatment of SAVf is based on endovascular embolization [10]. Because of the complexity of this case, different stage operations were performed. Go to:
Conclusions
CTA is very accurate and helpful in delineating anomalies like SAVf and atrial myxoma and in prompt management. Further study need to be done to explore any connections between them.
References:
1. Siablis D, Papathanassiou ZG, Karnabtidis D, et al. Splenic arteriovenous fistula and sudden onset of portal hypertension as complications of a ruptured spleni artery aneurysm: Succesful treatment with transcateter arterial embolisation. A case study and review of literature. World J Gastroenterol. 2006;12(26):4264–66. [PMC free article] [PubMed] [Google Scholar]
2. Madsen MA, Frevert S, Madsen PL, et al. Splenic arteriovenous fistula treated with percutaneous transarterial embolisation. Eur J Vasc Endovasc Surg. 2008;36:562–64. [PubMed] [Google Scholar]
3. Chhabra A, McClung JA, Kalapatapo S, et al. Giant myxoma causing heart failure symptoms. Am J Case Rep. 2012;13:29–32. [PMC free article] [PubMed] [Google Scholar]
4. Araoz PA, Mulvagh SL, Tazelaar HD, et al. CT and MR Imaging of Benign Primary Cardiac Neoplasms with Echocardiographic Correlation. Radiographics. 2000;20:1303–19. [PubMed] [Google Scholar]
5. Ibrahim WH, Bassurrah HM. Endovascular management of splenic arteriovenous fistula with giant venous aneurismal dilatation. Ann Vasc Dis. 2012;4:439–44. [PMC free article] [PubMed] [Google Scholar]
6. Chen B, Tang SW, Zhang CL, et al. Melena associated regional portal hypertension caused by splenic arteriorvenous fistula. World J Gastroenterol. 2012;18(16):1996–98. [PMC free article] [PubMed] [Google Scholar]
7. Gunther K, Stangl R, Schweiger H, et al. Post traumatic arteriovenous fistula between splenic artery and vein as a rare cause of acute myocardial ischemia. Chirurg. 1998;69:91–93. [PubMed] [Google Scholar]
8. Yadav R, Tiwari MK, Mathur RM, et al. Unusually giant splenic artery and vein aneurysm with arteriovenous fistula with hypersplenism in a nulliparous woman. Interact Cardiovasc Thorac Surg. 2009;8:384–86. [PubMed] [Google Scholar]
9. Grebenc ML, Rosade de Christenson ML, Burke AP, et al. Primary cardiac and pericardial neoplasms: radiologic – pathologic correlation. Radiographics. 2000;20:1073–103. [PubMed] [Google Scholar]
10. Crusco F, Antoniella A, Pulighedu C, et al. Post-operative splenic arteriovenous fistula detected with 16-multidedector computed tomography. Br J Radiol. 2007;80:216–18. [PubMed] [Google Scholar]